Friday, October 30, 2009
Saving Health Care--Saving America
Saving Health Care--Saving AmericaBy BRIAN KLEPPER, DAVID C. KIBBE, ROBERT LASZEWSKI and ALAIN ENTHOVENSo far, Congress' response to the health care crisis has been alarmingly disappointing in three ways. First, by willingly accepting enormous sums from health care special interests, our representatives have obligated themselves to their benefactors' interests rather than to those of the American
Latest Health Wonk Review is Up!
Yikes!
Tinker Ready of Boston Health News is at your door trick or treat with a well written, extensive and illustrated version of the latest Health Wonk Review. This one is all treat.
Check it out here.
Tinker Ready of Boston Health News is at your door trick or treat with a well written, extensive and illustrated version of the latest Health Wonk Review. This one is all treat.
Check it out here.
Thursday, October 29, 2009
More Implications on the Suspended Animation of the Medicare Medical Home Demonstration
 While most media and bloggery continue to glom incessantly over the iterations and implications of the ‘public option,’ the Disease Management Care Blog finds the suspended animation of the Medicare Medical Home Demo far more interesting.
While most media and bloggery continue to glom incessantly over the iterations and implications of the ‘public option,’ the Disease Management Care Blog finds the suspended animation of the Medicare Medical Home Demo far more interesting.As the astute Vince Kuraitis pointed out in this post, CMS' intentions are quite cryptic, the legal authority is opaque, plodding government demos can be outrun by the market and there’s a difference between demos (‘should we do this?’) and pilots (‘how can we do this?’). In prior posts (here and here), the DMCB also pointed out that a multi-payor collaboration offers up an important opportunity in experiential learning and could represent an important tipping point for the Medical Home.
What are other implications?
Medicare As A Continuous Learning Organization: Rigorously run demonstrations that compare one care approach versus usual care are ill-suited to finding out works in an environment of constant change and overlapping mutually supportive interventions in multiple geographies. This is CMS’ chance to realize an insight known to the population-based care community for years: when it comes to multi-dimensional care management, looking is not that same as seeing, listening is more important than hearing and knowledge pales in comparison to insight. The DMCB would like to be among the first to welcome CMS in from the oxygen-deprived academosphere.
First Among Equals: Not only are pilots broader in scope, the Vermont announcement suggests that future Medicare-owned medical home pilots will accommodate other insurers. These are typically fashioned as multi-payer ‘collaboratives’ (for example, here and here) that pool resources, share data, seek consensus and continuously adapt. How well Medicare can execute on this will depend on staffers who can be flexible and understand the difference between effectiveness and efficacy.
Government Silos: The DMCB has spoken to more than one Medicaid Medical Director who cajoled their States’ commercial insurers into participating in multi-payer medical home collaboratives. When it comes to government programs working with other payers, Medicaid’s clearly had a head start. Can Medicare and Medicaid just get along? We’ll see.
Boost to Accountable Care Organizations: Compared to Medical Homes, ACOs are far less defined, but the DMCB suspects they’ll be part of the coming health reform legislation. ACO’s will likely adopt Medical Homes along with all the other policy golden boys like electronic records, value-based purchasing arrangements and bundled payments. Look for CMS to use medical home collaboratives to ‘motivate’ multiple payers to support the embryonic ACOs until they’re able to prove their worth.
Start Building The Business Plans Now: Assuming a) multi-stakeholder pilots are flexible, b) can build on Medicaid’s as well as the commercial insurers’ positive experiences with disease management, c) care management resources can be shared among multiple primary care sites and d) many primary care sites will not want to reengineer what few nurses they have left, the future is very bright for organizations that know how to deploy trained, motivated and savvy nurses across a network. Here’s an example. More are undoubtedly on the way.
++++++
Addendum: e-CareManagement has another post on the topic that is well worth the read. Check it out.
The Health Care Bills, the Fine Print, and a Troubling List of Budget Gimmicks
Julie Appleby has an important article today at Kaiser Health News.She has identified an important and before unreported issue in the Senate Finance health care bill.In order to keep the cost of the plan down, the Senate Finance bill literally locks in the erosion of insurance subsidies for middle class families.From her report:"The first year the legislation would take effect, people getting
Wednesday, October 28, 2009
More on the Medicare Pilots: The Medical Home Purchasing Cartel That Includes Medicare
 What percent of the revenue or the patients is enough to get a hospital's or a physician's attention? In it's prior life in not-for-profit managed care, the Disease Management Care Blog was stymied by only 'owning' a low percent of the patients in many of the provider settings. As a result, even if there were important quality initiatives backed-up by serious money or free assistance (usually in the form of care management nurses), the lack of critical mass compared to other payers hampered our ability to get anything done.
What percent of the revenue or the patients is enough to get a hospital's or a physician's attention? In it's prior life in not-for-profit managed care, the Disease Management Care Blog was stymied by only 'owning' a low percent of the patients in many of the provider settings. As a result, even if there were important quality initiatives backed-up by serious money or free assistance (usually in the form of care management nurses), the lack of critical mass compared to other payers hampered our ability to get anything done.Which is why the Vermont CMS Demo i.e. pilot on involving a multi-payer collaborative in support of the medical home, is so important. By having the all the key purchasers of medical services form a medical home cartel i.e., monopsony, the providers will have to pay attention. The providers will also 'win' by having to operationally deal with single set of processes and payment mechanisms. Last but not least, Medicare (ironically) will be kept honest, because it will have to adapt some of its operations to mirror those of the other more experienced payors. Think tipping point leading to a virtuous cycle.
That's also called synergy, which is why a multi-stakeholder pilot - assuming CMS can collaborate - will be far more likely to show positive outcomes that a single Medicare demo.
how cool is this?

Yesterday morning, I got a call from Oresta. She told me that she had read my article in the Centretown Buzz and wanted to reach out to me.
Even though I love her store and spa (I asked for gift certificates for Christmas last year), I was not on her mailing list and had not received the letter that I posted above.
It's hard to read, so here is the text, in full:
OCTOBER is BREAST CANCER AWARENESS MONTH
Pinkwasher: (pink’-wah-sher) noun. A company that pur-
ports to care about breast cancer by promoting a pink
ribboned product, but manufactures products that are
linked to the disease.
Dear clients,
ORESTA organic skin care confectionery is committed to providing organic spa
treatments and to supporting companies that manufacture truly pure and organic
products. We believe in beauty without compromising your health.
We have been touched by cancer in our families and with our clientele - as
cancer survivors and undergoing cancer therapy. The prevailing comment of clients
who have come in for a spa treatment while undergoing therapy was how nurturing a
visit to ORESTA organic skin care confectionery was for them.
We have wanted to help the cause but have struggled with a way to do this.
Do we donate a % of sales? a % of services? Do we fundraise? For which organiza-
tion or foundation? In the end, what feels right for us, is doing what we do best:
pampering.
If you, a friend or loved one is undergoing cancer therapy and would enjoy an
organic facial treatment, please contact us. We are committed to treating one
woman per week to a complimentary ORESTA treatment.
Oresta was calling to offer me a facial (I am going on Friday) but I offered to blog about this offer. She asked me to clarify that she and her staff will be offering this service to women undergoing treatment throughout the year - not just during October.
I am impressed and touched beyong words. Have any of you ever heard of anyone else doing this?
I told my spouse that, by coincidence, I had written in journal that morning that I would really like a facial. He said, "Tomorrow, could you write that you would really like a home renovation?"
Tuesday, October 27, 2009
Medicare Medical Home Demo Cancelled. Medicare Medical Home PILOTS Are On The Way
 In a prior post, the Disease Management Care Blog broke the news that the Medicare Medical Home Demonstration had been placed on perma-hold by CMS. The announcement is now official, and you can read all about it and many of the implications at Vince Kuraitis' e-CareManagement Blog.
In a prior post, the Disease Management Care Blog broke the news that the Medicare Medical Home Demonstration had been placed on perma-hold by CMS. The announcement is now official, and you can read all about it and many of the implications at Vince Kuraitis' e-CareManagement Blog.As pointed out in e-CareManagement, the purpose of a 'demo' is to ask 'if' a patient care intervention works, usually by comparing the outcomes of the patients in the intervention group to the outcomes of patients in a parallel control group. The Medicare Medical Home Demonstration is being effectively cancelled because the House Bill 3200 proposes a Medical Home 'Pilot' Program. The DMCB interprets the purpose of a pilot is to ask 'how' a patient intervention works. 'If' is first generation Ver. 1.0. 'How' is second generation Ver. 2.0
How could medical home 'pilots' be conducted by CMS? One big hint lies in the Green Mountain State, where the Secretary of HHS announced that Medicare will participate in a 'multi-payer' 'demo' evaluation. Don't let the word demo fool you. The bad news is that the multi-payer dimensions of this initiative will complicate any formal and traditional assessment of the impact of the medical home for fee-for-service Medicare beneficiaries. The good news is that this looks and feels like a pilot in which CMS will gain a treasure trove of experience on making the medical home 'work' in the real world.
chemotherapy and the H1N1 vaccine
As someone in ongoing chemotherapy, I have a compromised immune system. This puts me at increased risk for contracting H1N1.
I am among the priority groups established by the City of Ottawa, as is my family, and were it not for the hours long lineups (several centres closed the lineups by late afternoon), I would have had my shot yesterday.
I did call the oncologist yesterday to ask about interactions between Neupogen (the drug I take after chemo to boost my white blood cell count and fight infection). When I didn't hear back immediately I checked with the cancer centre receptionist who, told me (after checking with someone) that I should go ahead and get the shot.
Today, the nurse who works with my oncologist called and told me to wait.
The reasoning goes as follows:
Chemotherapy suppresses the immune system.
The flu shot is meant to boost it.
Having the H1N1 shot (or any other flu vaccine) too close to chemotherapy lessens the effectiveness of the shot.
Those of us getting chemo are instructed to wait to the end of the chemo cycle, get our bloodwork done (to ensure that our counts are high enough) and then get the shot the day before the next round of chemo.
This means that I will be waiting until November 10 for my H1N1 vaccine.
And washing my hands. A lot.
Monday, October 26, 2009
The Guerrilla Approach to the Care Management that Underlies the Patient Centered Medical Home
 At a recent webinar, the Disease Management Care Blog was asked how a regional health insurer implement a medical home if its provider network a) is dominated by small physician practices and b) there are no State-wide multi-payer-provider initiatives underway.
At a recent webinar, the Disease Management Care Blog was asked how a regional health insurer implement a medical home if its provider network a) is dominated by small physician practices and b) there are no State-wide multi-payer-provider initiatives underway.The DMCB at your service.
When it looks at what's been written about the core elements of the patient centered medical home, one recurring theme is the role of non-physician professionals - typically registered nurses - providing face-to-face (as well as remote telephonic) care management. The ingredients of that care management include patient engagement in the mangement of their own illness, coordinating that management with the primary care physician, acting as a primary point of contact for other members of the health care team as well as outside consultants, helping the patient to extract maximum value from the insurance benefit and maintaining and documenting an ongoing care plan.
Therefore, the guerrilla approach to creating care management to is for the insurer to establish that nursing resource for themselves.
Based on what it's heard on the non-Medicaid 'street,' the DMCB assumes that would involve a retail cost of anywhere from $20 to $50 per enrolled patient per month. Assuming that's true, it would dedicate most of that cost to the nurses' salary and benefits but take a fraction and give it to the physicians in exchange for letting the nurses into the practice. The DMCB is no business person, but a back of the envelope calculation suggests that each nurses would have to carry from 150 to more than 200 patients to cover their salary and benefits. There's some additional cost including the use of a car and laptops. The DMCB thinks the nurses would need to be distributed geographically and serve a hub of primary care sites, starting with the clinics that serve a large proportion of the insurer's patients.
Readers are probably thinking about the likelihood of getting this kind of sticker shock past the Chief Financial Officer. Yes, it IS pretty low, but you have several options: 1) argue that you'll only enroll patients that are likely to have $20-$50 in reduced claims expense thanks to the care management nurses' interventions, 2) sell the increased premium expense to customers that want a 'medical home' in their network (and that Medicare Advantage will use a bonus mechanism to cover that cost), 3) extract that cost by reducing payments for other services or 4) recognize this is a cost of doing business in an environment that demands the medical home all with or without the option of hiring a richly paid consultant (hint from the DMCB spouse).
The DMCB suspects some physicians will simply refuse to let a nurse into their practice. Other physicians will demand to hire their own nurse in exchange for the option of collecting the entire fee of $20-$50 PMPM. Fine, says the DMCB, but it would want to see a care management job description connected to a live care manager and have the option of performing an audit of the care plans.
Last but not least, the DMCB understands there are other elements of a medical home such as decision support, an electronic record, creating policies, NCQA recognition and 'transforming' the primary care site. While those other elements bring additional value, the purpose of hiring the nurses is not to establish 'medical homes,' but to create the greatest value proposition of medical homes: nurse-led care management.
The secret sauce here is the background, skill set, attitude and personality of the nurses. They need to understand outpatient primary care, appreciate the importance of patient engagement, buy into the notion of bridging the primary care-insurer divide and be smiling and steely-nerved ambassadors.
By the way, yes, that's a picture of Flo Nightingale above after her return from the Crimean front. Take away the bullets, and the DMCB sees many similarities between her role then and the new role demanded of nurses in the battle against chronic illness.
“The Public Option Is Back in Play”—That Depends Upon Your Definition of the Word “Is”
It appears that Harry Reid is going to include a robust Medicare-like public option in his Senate draft. Speaker Pelosi is also doing her best to put as robust a public option in her House version as she can get the votes for.One press report after another has proclaimed the return of the public option.I’d like to see some of these reporters to do a vote count.No doubt the hype over the public
Sunday, October 25, 2009
H1N1 Vaccination: The Difference Between the Obama Administration Being At Fault and Being Responsible
_svg.png) The Disease Management Care Blog has pointed out twice (here and here) that the Obama Administration's health care chops will be tested by H1N1. The President can't blame a lack of any warning, the prior Republican administration, absent regulations or an unfunded infrastructure. While moving virus from eggs to humans is very complicated, this is a public health effort that risks falling short across the entire system bandwidth of health care - most visibly the part owned by the Federal government.
The Disease Management Care Blog has pointed out twice (here and here) that the Obama Administration's health care chops will be tested by H1N1. The President can't blame a lack of any warning, the prior Republican administration, absent regulations or an unfunded infrastructure. While moving virus from eggs to humans is very complicated, this is a public health effort that risks falling short across the entire system bandwidth of health care - most visibly the part owned by the Federal government.Of course, there is no underestimating the capacity of loonies on the left or the right and the middle to refute the same technology that conquered small pox and polio. The community-dwelling DMCB personally discovered this nuttiness is not confined to distant enclaves and AM radio. The astonished DMCB ran into one urbane and educated colleague who, over a glass of Toasted Head, serenely discounted the research on vaccines. No amount of explanation could get past his blinkered anti-science puritanism.
Whatever. Americans still have the right to make bad decisions.
What the DMCB worries about, however, is that those who correctly decide to get the vaccine won't be able to get it, those unable to get the vaccine will get ill, those who are ill won't be able to get to a physician, those unable to get to a physician will overwhelm emergency rooms, and those in the emergency rooms will overwelm the hospitals. It won't necessarily by the White House's fault, but given their leadership and visibility in this area, they will be held responsible.
Fairly or not, the risk is that opponents of health reform will use a failed vaccination campaign to impugn the Obama Administration's competence in managing the nation's health. The DMCB wonders if this could reduce the odds that legislation will be passed.
Friday, October 23, 2009
beautiful night
Thanks to everyone who came to the Toronto launch last night.
My face hurts from smiling and my heart is so full it could burst.
And the bookstore sold out the books.
My face hurts from smiling and my heart is so full it could burst.
And the bookstore sold out the books.
Labels:
books,
Breast Cancer,
good stuff,
joy,
travel,
writing
Thursday, October 22, 2009
Observations About Today's Patient Centered Primary Care Collaborative Annual Summit. Most Important: The Value of Magic Nurse Stuff.
 The Disease Management Care Blog spent an extremely rewarding day at the Washington DC Primary Care Patient Centered Collaborative's Annual Summit on the Patient Centered Medical Home. It caught up with colleagues, got some valuable scientific updates and got to share in the growing enthusiasm for a very compelling approach to care. It also grabbed a copy of this report that was released today, 'Proof In Practice,' that will be the topic of a future DMCB post.
The Disease Management Care Blog spent an extremely rewarding day at the Washington DC Primary Care Patient Centered Collaborative's Annual Summit on the Patient Centered Medical Home. It caught up with colleagues, got some valuable scientific updates and got to share in the growing enthusiasm for a very compelling approach to care. It also grabbed a copy of this report that was released today, 'Proof In Practice,' that will be the topic of a future DMCB post.Random observations from today's meeting in no particular order:
This time the PCPCC Meeting was held in a very large room in the Washington DC Convention Center. There were over 400 attendees and the crowd was very supportive. The Patient Centered Medical Home appears to have gained considerable momentum - and that's putting it mildly.
Several Congressional staffers were there along with a House Representative who gave the keynote. Based on their comments, it's pretty clear that some version of the PCMH will be in the final health reform bill. The DMCB suspects that 'pilots' will be used in lieu of 'demonstrations' in FFS Medicare. In D.C.-speak, pilots have a better open-ended political prognosis than 'demonstrations.'
One key Congressional staffer pointed out that there seem to be many iterations of the PCMH ('means different things to different people') with variable outcomes ('for example, it doesn't consistently reduce repeat hospitalizations'). While some prefer to 'lump,' Congress is leaning toward 'split' by recognizing two models of the medical home: 1) 'high intensity' and 2) 'low intensity.' Each warrant different levels of funding support. Watch for this in the final health reform bill.
One physician audience member pointed out that his Medicare Advantage (MA) Plan has been offering a version of the PCMH for years. He pointed out that if MA funding is cut, this could mean its demise. The panel responded by noting that most MA Plans have not used their allegedly high fees to support versions of the PCMH. In response, MA funding cuts are politically inevitable, but there is a chance that bonuses will be offered to MA Plans that offer care coordination. Look for this in the final health reform bill also.
Why aren't commerical insurers and self-insured employers stampeding toward the PCMH? Three reasons were offered: 1) the PCMH is very much a function of managing 'locations' in a network that depends on local physician adoption; it's easier to just manage the benefit design, 2) it's still all about a short term focus on costs, not a long term emphasis on 'value,' and 3) irrefutable and solid 'proof of concept' is still lacking.
That's not stopping the Veteran's Administration. All 820 of their primary care sites are going to be transformed to PCMHs over the next two years thanks to a combination of experiential learning collaboratives, learning colleges, consultation teams, demonstration labs and an abundance of communication. The VA's challenges are 1) promoting 'top of license' care among members of the PCMH team, 2) limited phone based care experience, 3) the usual challenges in retooling for chronic care activities, 4) limited experience in managing transitions between the hospital and the outpatient setting, 5) while the VA's EHR is robust, its decision support capabilities are minimal.
Last but not least, much of what appeared in the many panel discussions and on screen in the PowerPoints was filled with nursing concepts and terminology. To the DMCB, it's pretty clear that the core of any PCMH is high-end primary care nursing. Sure, we need physician leadership, information technology, teaming, payment reform etc, but let's face it: when it comes to assembling and managing the resources necessary to care for patients with chronic illness, physicians can best lead by getting out of the way. To us docs, it's magic nursey stuff. The good news is that it seems to work not matter what you call it and that the nursing profession is finally going to get the recognition that it deserves.
Doing the Right Thing--The Doc Fix Vote and the CMS Report
Predicting the outcome of yesterday's Senate vote on the $245 billion deficit adding doc fix was easy.Democratic Senate Majority Leader Reid was going to sail this thing through the Senate with almost all Democrats and even a bunch of Republicans onside.Senators are afraid of the docs—after all they have voted for years to waive any cuts. Democrats needed to get this $245 billion cost out of the
News About the Medical Home Demo
The Disease Management Care Blog understands that it has been decided that it would be impractical to clear the Medicare Medical Home Demonstration, which has been under review at the Office of Management and Budget, given the pending legislation that would repeal it and replace it with a similar pilot. You read it here first.
launching
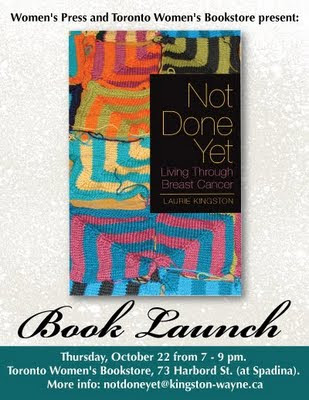
I'm off to Toronto today to celebrate my book! If you're in town, come see me at the Toronto Women's Bookstore.
We'll have a little nosh, a little drink, I'll read from the book...I think it will be a nice evening.
Meanwhile, here's a link to a blog called "Incredible Women," where I am honoured to say that I am being featured today.
Labels:
blook,
Breast Cancer,
community,
good stuff,
joy,
lucky,
travel
Wednesday, October 21, 2009
 While a New England Journal of Medicine article on a poll showing high physician support for Massachusett's health insurance reforms* captured some of the news cycle, the Disease Management Care Blog was much more interested in catching up with this jewel from a week earlier on the logic underlying Medicaid's inclusion in healthcare reform.
While a New England Journal of Medicine article on a poll showing high physician support for Massachusett's health insurance reforms* captured some of the news cycle, the Disease Management Care Blog was much more interested in catching up with this jewel from a week earlier on the logic underlying Medicaid's inclusion in healthcare reform.This article by George Washington University academician Sara Rosenbaum is a very handy and well written summary. Recall that Medicaid covers a whopping 60 million Americans that generally meet three broad conditions: 1) age (children and the elderly), 2) a qualifying condition (pregnant, disabled or a caretaker of children) and 3) income (a percent of the Federal Poverty Level or FPL). The latter category threshold varies from State to State (from a low of 17% to a high of 275%). The first two conditions trump the latter. If you are a ‘nonelderly’ adult and don’t have a qualifying condition, you are out of luck when it comes to Medicaid no matter how low your income is. You probably can't afford commercial insurance either, which means you are uninsured.
That may change thanks to the bills before Congress. They bascially do two things: 1) eliminate the age/qualifying condition barriers, and 2) create a one size income standard as a percent of the FPL across all States.
Fans of the private market may wonder why health reform is turning to Medicaid. According to the article, it is more than just a matter of the Democrats’ policy preferences.
First of all Medicaid is the cheaper alternative. States are required to cover part of the Medicaid budget, Medicaid has a lower fee schedule and its administrative costs are partially carried by the government. Private insurers can't match this. Ms. Rosenbaum quotes research showing comparative policies for private insurance could cost approximately $6000 while Medicaid’s cost would be less than $2000. That’s over 4000 reasons in favor of Medicaid.
Secondly, absent highly vigilant and extensive regulation, the private market could easily tilt toward ‘cherry picking’ and actively enroll a younger and healthier population. Medicaid programs, in contrast, are configured to be a fiduciary for the poor and ill without any of the enrollment or benefit gamesmanship.
Last but not least, the professionals that administer Medicaid understand the special needs of persons living at the margins of society. They understand how community health centers, public hospitals and local agencies can be used to best serve underserved persons living in inner cities or rural settings. This kind of expertise is simply unavailable in the commercial insurance market.
The article closes with three 'show me the money' recommendations:
1) Show me (the States) the money. Without credible support from the Feds, the States may be simply unable to afford their share of an expanded Medicaid program.
2) Show me (the docs) the money. Without credible support from the Feds, the States may simply squeeze their payment rates down to unsustainable levels. Spotty physician refusal to accept Medicaid patients could uptick considerably.
3) Show me (the system) the money. Medicaid needs to become more a visible player in each of the States' efforts to rationalize health care, increase quality and drive greater value.
Readers may or may not agree with the rationales described above, but they make sense from an insurance reform perspective. Unfortunately, other than reducing benefits and lowering payment levels, the DMCB sees few other options for a new and improved Medicaid to hold down costs if health care inflation continues unabated.
++++++++++++++++++
*The DMCB cannot resist. Of course physicians prefer it when their patients have an ability to pay for health care services. Check out this telling article on the Brit's introduction of the National Health Service in the 1940's and politician Nye Bevan's "bribe" to win the support of the physician consultants: "I stuffed their mouths with gold."
milestone reviewed
I am featured on a blog called "Women at Forty" today.
When I was aked to submit a post, I thought it would be appropriate to re-visit a post I wrote on the eve of my fortieth birthday.
I'm looking forward to writing my fiftieth birthday post. Only eight more years and countless clean scans to go.
The Latest Cavalcade of Risk is Up!
Boo!
Frightened by all the bad risk out there? Your money could evaporate, your good health could vanish, your car could crash or your employees could go absent. Learn how to think about this and more at Lynch Ryan's Cavalcade of Risk's spooky pre-Halloween edition.
Frightened by all the bad risk out there? Your money could evaporate, your good health could vanish, your car could crash or your employees could go absent. Learn how to think about this and more at Lynch Ryan's Cavalcade of Risk's spooky pre-Halloween edition.
Tuesday, October 20, 2009
The Genetic Information Nondiscrimination Act (GINA), Health Risk Assessments (HRAs) and Lawyers Run Amok
 The Disease Management Care Blog received a DMAA email containing this press release today. It calls for a moratorium in "GINA regulation implementation."
The Disease Management Care Blog received a DMAA email containing this press release today. It calls for a moratorium in "GINA regulation implementation."What's this about you ask? The DMCB at your service.
GINA is part of the logarithmically expanding blob of Washington D.C. acronyms. This particular one refers to the 'Genetic Information Nondiscrimation Act' that was signed into law by President Bush on May 21, 2008. Its intent was to prevent discrimination based on genetic information by health insurers and employers.
In reading about the act here, it appears that the way discrimination is prevented is by prohibiting employers and health insurers from collecting any genetic information in the first place. In addition to not collecting it, insurers are also prohibited from using it for decisions about coverage or rates (by insurers) or for hiring, firing, promotions or other decisions about the terms of employment (employers).
So far so good.
So the intrepid DMCB went to the text of the law itself and found a lot of language stating that collecting and use of 'genetic information' was prohibited in health insurance 'underwriting.' The statute has very clear definitions of underwriting ('health insurance rules used to determine eligibility, computation of premiums, exclusions of pre-existing conditions and other activities related to contracting health benefits') and genetic information ('results of genetic tests of the individual or the family members and the manifestation of a disease or disorder in family members of an individual').
The DMCB is struck by the inclusion of 'family history.' Read on and you'll see why.
On Oct 7, 2009, the Departments of Labor, Treasury, HHS and the Equality Employment Opportunity Commission released proposed regulations a.k.a interim final rules that are intended to guide their interpretation and enforcement of GINA. The rules become effective on December 8, 2009.
The lawyers that crafted these regulations must have also been struck by the term 'family history,' because they've addressed it in the context of health risk assessments (HRAs).
HRAs are widely used in the population-based health care. It typically consists of questionnaire that asks a series of health related questions. The individual answers can then be summed up to determine an overall risk score in one or more health domains. This is an example of an HRA used to assess the risk from being overweight, while this HRA determines the risk of future heart attack. Note that both of these examples include family history as one factor in the overall assessment of risk.
What do the interim final rules say? They correctly point out that HRAs that include family history questions are typically distributed at the time of new or re-enrollment and are often accompanied by incentives to complete the survey. When present, these incentives consist of rewards such a premium reductions, lower deductibles and cash bonuses. Since this is money that is tied to the premium which is defined to be part of underwriting, the practice will become illegal on December 7.
What's more, if the HRA is requested prior to enrollment, even if there is no payment to the enrollee, the act of collecting the 'genetic information is also a violation of the law.
If your disease management organization, population-based care company, employees benefit plan or health insurer uses HRAs at the time of open enrollment, you have two choices:
Change how the HRA is done: No financial incentives, period. What's more, the HRA can't be distributed or collected until after enrollment,
or
Strip all the family history questions out of the HRA.
The DMCB agrees with the DMAA that the interim rules need to be put on hold until this twisted pretzel logic of lawyers run amok is straightened out.
First of all, while inquiries about family history can be intrusive to individuals completing HRAs, the cash value of the incentives are undoubtedly very welcome and are a fair value transaction.
The DMCB also did a word search of the original statute and did not find the term 'health risk assessment.' It doubts our legislators intended to sweep HRAs into the scope of this legislation.
It is also illogical to group the practice of increased payment to all enrollees with and without significant family histories with the other repugnant practices of charging more or denying benefits on the basis of genetic history. The resemblance is superficial to anyone with common sense.
In addition, in real practice, it is highly unlikely that the underwriters in any health plan would harvest the data from HRAs and mathematically price it into their premium decision-making. It is theoretically possible, but that's simply not how the business is operates.
Last but not least, the risk of harm from showing some flexibility around this topic is far less than the risk of harm from hobbling how HRAs are distributed, completed and used. Thanks to HRAs, companies are not only extending hard cash but using the information to provide a higher level of service to individuals who would benefit from it.
If the DMCB is reading things right, comments on this silliness can apparently still be submitted (E-OHPSCA.EBSA@dol.gov) through January 5, 2010. The DMCB copied the above text and simply emailed it in over its signature.
de-bunking the pink
"Three years ago, I saw a story on the news while I was at the gym. An investigative feature on the breast cancer awareness contributions that various corporations pledged during Breast Cancer Awareness Month found that most of these promotions led to increased sales and windfall profits that dwarfed the piddling donations that the extra sales generated. Until that moment, I was gung-ho about buying products marked with pink ribbons."
And so begins the best article I have ever read on the subject of the pink-washing of October (and not just because the author says you should all go out and buy my book). Suzanne Reisman hits all the bases in this piece and does it with eloquence and a sense of humour.
If you have ever struggled to understand why some of us object to pinxploitation (I just made that word up), your questions will be answered.
Monday, October 19, 2009
Medicare For All, i.e., the Public Option Can Cause Cost Shifting. It Is Possible.
 Commercial health insurers are arguing that a government run ‘public option,’ if included in health reform, will force a take-it-or-leave-it’ low-ball fee schedule on hospitals and physicians. This, in turn, will lead the providers to recoup their losses by charging the competing private insurers correspondingly more for the same services. This phenomenon is known as ‘cost shifting.’
Commercial health insurers are arguing that a government run ‘public option,’ if included in health reform, will force a take-it-or-leave-it’ low-ball fee schedule on hospitals and physicians. This, in turn, will lead the providers to recoup their losses by charging the competing private insurers correspondingly more for the same services. This phenomenon is known as ‘cost shifting.’Various luminaries have dismissed this as pernicious (former Secretary of Labor Robert Reich) a misrepresentation (Nobel Prize winning Paul Krugman) and taxing credulity (Princeton health care economist Uwe Reinhardt). Absent any data that prove that this really happens, critics of the evil, recessioning, care-denying and robber baron health insurers charge there they go again: they’re trying to pull a fast one on the unsuspecting public.
In its past life in the managed care industry, the Disease Management Care Blog remembers hospital administrators repeatedly arguing that they needed the commercial insurers to pay their institutions higher rates than Medicare to remain in business. Since Robert, Paul and Uwe suggest this was just a negotiating ploy, the DMCB did what it usually does when it’s confused. It looked at some peer-reviewed literature.
It didn’t take much to find three articles in a health policy journal named Health Affairs that is not known for excess partisanship or biased authors.
This 2003 article by Lee and colleagues points out that when Medicare’s DRG payment system ‘gets it right,’ by correctly paying hospitals, there is no need for hospitals to cost shift. The authors seem to imply that when Medicare underpays hospitals, they turn to cost shifting to make up the difference.
In this 2003 article, Paul Ginsburg argues that there is a lack of evidence of the phenomenon but, on theoretical grounds, it is quite possible to assemble a ‘conceptual basis’ for cost shifting. He shows it can certainly happen in geographic areas where one health care provider has market dominance and the health insurers have no choice but to agree to their terms. In the DMCB’s experience, this monopolistic behavior is common in rural areas where there is only one hospital per county, or anywhere when a medical specialty’s services (like high end cardiology) are otherwise not available.
In this 2006 article Jack Zwanziger and Anil Bamezai examined the relationship between Medicare and Medicaid rates versus private insurance rates in California and found an inverse financial correlation in rates to the tune of a 0.17% increase for every 1% decrease by Medicare. While the relationship is not necessarily causal, the association suggests that the phenomenon of cost shifting is real. It's not dollar for dollar, but the 'signal' was out there.
The DMCB concludes that cost shifting is quite possible under the public option. It also wonders if it is missing something and why such smart people are so dismissive of any likelihood that it could happen.
advice (with the benefit of hindsight)
Last week, the Centretown Buzz (an Ottawa community paper) asked me to write the article that "I wish I could have read when I was first diagnosed."
It's on the front page of this week's issue, and begins like this:
As I looked back on the last few years, the following key points best summarize my advice:
The entire article is online, so you can read it for yourself.
Let me know what you think. And if you've been there, please don't hesitate to share some of your hard-earned experience.
It's on the front page of this week's issue, and begins like this:
On December 1st, 2005, I found a lump in my breast, as I was getting undressed. One month later, I was diagnosed with breast cancer. I was 38 years old, with two young kids and a very hectic life. I felt completely blind-sided.
Almost four years later, and with the benefit of hindsight, I share some advice for others who find themselves in my situation.
As I looked back on the last few years, the following key points best summarize my advice:
Bring someone with you to appointments, especially in the beginning.
Be your own advocate.
Be nice to the admin staff and nurses.
Don’t compare yourself to anyone else.
Let others help you.
Never give up hope.
The entire article is online, so you can read it for yourself.
Let me know what you think. And if you've been there, please don't hesitate to share some of your hard-earned experience.
The Senate Finance Insurance Reform Rules Have to Be Fixed in Spite of the Gang That Can’t Shoot Straight
Last week the health insurance trade association (AHIP) released a report it sponsored, and was authored by PricewaterhouseCoopers (PwC), that claimed the Senate Finance bill would be problematic for the insurance markets only leading to much higher costs.As I posted last week, my own analysis of the Finance bill gives me big concerns about what it would do to health insurance costs and the
Sunday, October 18, 2009
Comparing and Contrasting Population Health/Disease Management and the Patient Centered Medical Home
 The Disease Management Care Blog has given a number of grand rounds, webinars and presentations and, like many speakers, has a core set of PowerPoint slides that seem to make it into every occasion. In thinking about it's last few engagements, one slide in particular keeps cropping up. It's a fav that compares and contrasts six key domains of the population health née disease management and the patient centered medical home.
The Disease Management Care Blog has given a number of grand rounds, webinars and presentations and, like many speakers, has a core set of PowerPoint slides that seem to make it into every occasion. In thinking about it's last few engagements, one slide in particular keeps cropping up. It's a fav that compares and contrasts six key domains of the population health née disease management and the patient centered medical home.Who: In population health (PH), it's the nurse-coach manager who is engaging the patient. In the PCMH, that role belongs to the primary care site-based team that includes a nurse-care manager.
What: In PH, the 'what' is an enabled, confident patient who is better able to participate in decision making. In the PCMH, it's all about the patient ideally becoming a member of the health care team in mutual decision making.
Where: In PH, it's remote and virtual. In the PCMH, it's local and based on the 'bricks and mortar' of the primary care site.
When: i.e., when do I see my money? In PH, the money is based on a year-end reconciliation of the observed vs. the expected costs i.e., savings. In the PCMH, there may be some upside gain sharing and/or P4P at the end of the year, but the real money is paid every month on a risk adjusted basis for every person that is enrolled, i.e., revenue.
Why: The lingering success of the disease management organizations makes the DMCB think that why is a function of the market still demanding PH. In contrast (pending data on the ROI from the PCMH pilots), the why is a function of policy making and the belief that it will play an important role in the resurrection of primary care.
How: In PH, change is accomplished by activating and engaging patients, who are then empowered to deal with the health care system based on their own goals and values. In the PMCH, change is accomplished by fundamentally altering the practice of primary care.
The DMCB agrees that the PH-PCMH overlap is far greater than any real differences.
The DMCB would be happy to share the slide. Just email 'n ask.
Thursday, October 15, 2009
The Sauce vs. Soufflé Approach to Care Management: Implications for Health Reform
 Thanks to all those cooking shows, the Disease Management Care Blog fancies kitchen metaphors. In thinking more about yesterday’s post on ‘care management,’ one allegory came to mind: the making of sauces versus soufflés. It occurred to the DMCB that care management, despite all the scientific trappings, is best thought of as a sauce. How well health reform can swallow that remains to be seen.
Thanks to all those cooking shows, the Disease Management Care Blog fancies kitchen metaphors. In thinking more about yesterday’s post on ‘care management,’ one allegory came to mind: the making of sauces versus soufflés. It occurred to the DMCB that care management, despite all the scientific trappings, is best thought of as a sauce. How well health reform can swallow that remains to be seen.When the DMCB makes spaghetti sauce, it knows the red stuff basically involves tomatoes. Once that basic ingredient is fulfilled, the rest is a creative mix of spices, maybe some wine, chopped sweet peppers, mushrooms, onions, garlic, other stuff and what-the-heck whatever-this-is-from-the-fridge and then drinking some wine. Think The Godfather’s Peter Clemenza and his famous going to the mattresses recipe for 20 guys.
Then there are soufflés. The closest the DMCB ever got to that level of culinary expertise was when it tried to make crème brûlée. What unfolded early the next morning wasn’t pretty. The point is that the DMCB appreciates that soufflés require an extraordinary level of cookery. The ingredients have to be apportioned in exact amounts, their mixing has to be precise and the oven temperature and bake time must be unerring or the result will be a stone. In medicine, think the operating suite and making sure the same check list is completed all the time every time.
When guests sit down to the DMCB’s sauce n’ pasta, they know what it is and it usually does the job. In the world of case management, the red stuff (otherwise known as the key core ingredient) is the generalist registered nurses referred to in Dr. Bodenheimer’s New England Journal article on care management. The rest is based on nursing science, lots of opinion, local culture, available resources and what’s in the fridge.
Check out the peer-reviewed literature used by Dr. Bodenheimer to make the case for care management. There is one reference on advance practice nurses and the role they play in helping patients discharged from six city hospitals, another on ‘trained nurses’ using a Care Transitions protocol for recently discharged patients in Colorado and primary care-based registered nurses in Baltimore who had completed a course in ‘Guided Care Nursing .’ There are other examples used in the article, including a geriatrician-led high risk clinic doing home visits, a roving geriatric physician-two nurse team managing 300 patients and the CMS capitated benefit plan called PACE. All are unique, yet all share the key ingredient of nurses doing nursing stuff that help patients move from point A to point B. It’s what does the job.
In the DMCB’s recent American Journal of Managed Care editorial, it argued that population-based programs for the care of patients with chronic illness are necessarily varied. The core ingredient makes it recognizable but around it there is considerable creativity and flexibility. Dr. Bodenheimer’s article didn’t necessary address the non-uniformity of care management, but the references he used certainly speak to that dimension.
As a result, it will be very challenging for accreditation agencies, recognition programs, managed care and accountable care organizations as well as Federal health reform and all the necessary regulations that follow to accommodate all those excellent cooks and their wonderful savory creations in the delivery of care management. Hopefully, the powers-that-be will recognize the need for flexibility in this area.
Hopefully, they'll be less about soufflés and more about sauces.
+++++++++++++++++++++++
Post script: The closest Dr. Bodenheimer has come to endorsing disease management is also in this New England Journal article:
'Telephonic care management has been effective when combined with face-to-face visits but has not worked by itself.'
Welcome to the club, Dr. B. The DMAA's been pointing this out for over a year and regular readers of the DMCB have long been familiar with the concept.
Apparently The "Games" Have Begun--Democrats Move to Fix Physician Fee Problem Off-Budget
Apparently, Democrats are getting ready to pay-off the physicians for their support of the health bills by quickly fixing the Medicare Sustainable Growth Rate (SGR) fee cut problem off-budget and ahead of the pending health care bills.This in today's Kaiser Health News on a Congress Daily Report:Physician lobbyists met with several key lawmakers and administration officials Wednesday to push for
The Latest Health Wonk Review Is Up
That's right, the latest and the bestest from the health care-related blogs, giving insights unavailable anywhere else is up at Hank Stern's Lean Mean and Clean summary. He calls it like he sees it, has nice things to say about the DMCB and as an extra bonus, throws in a pun. This prose by any other name smells as tweet!
will you be there?
Just a reminder to anyone who lives in Toronto or anywhere nearby or who would like to visit Toronto that my book party (postponed in June because of the flu) has been re-scheduled for October 22, from 7-9 pm.
I have been washing my hands lots and lots so that this overdue celebration can happen.

Also, I have been getting lots of interesting comments and messages in answer to my post on internet community. It's not too late to jump into the discussion.
I have been washing my hands lots and lots so that this overdue celebration can happen.

Also, I have been getting lots of interesting comments and messages in answer to my post on internet community. It's not too late to jump into the discussion.
Wednesday, October 14, 2009
The Definition of 'Care Management' Courtesy of the New England Journal
 The Disease Management Care Blog appreciates it when a useful definition appears in the peer-review literature. It helps everyone in the population-health care business to agree on terms, concepts and principles. The definition of 'care management' has now appeared in an article* by Thomas Bodenheimer and Rachel Berry-Millett in the Sept. 30 New England Journal of Medicine. This quote and the reference can be used by population health warriors everywhere who are dealing with those upcoming responses to RFPs, business plans, presentations, learning sessions, staff meetings, PowerPoints, professional development classes and care initiatives:
The Disease Management Care Blog appreciates it when a useful definition appears in the peer-review literature. It helps everyone in the population-health care business to agree on terms, concepts and principles. The definition of 'care management' has now appeared in an article* by Thomas Bodenheimer and Rachel Berry-Millett in the Sept. 30 New England Journal of Medicine. This quote and the reference can be used by population health warriors everywhere who are dealing with those upcoming responses to RFPs, business plans, presentations, learning sessions, staff meetings, PowerPoints, professional development classes and care initiatives:Care management is a set of activities designed to assist patients and their support systems in managing medical conditions and related psychosocial problems more effectively, with the aims of improving patients’ functional health status, enhancing the coordination of care, eliminating the duplication of services, and reducing the need for expensive medical services.
There have been other definitions (for example, here and here) and they more or less support the same concepts, but this may turn out to be the oft-cited reference because:
a) let's face it, it's in the New England Journal. It looks good when you quote it.
b) the authors explicitly point out that care management is generally provided by a 'registered nurse.' The DMCB heartily agrees because it is a big fan of nurses and has witnessed repeatedly how their common sense and familiarity with the 'system' are invaluable to docs and patients alike. What's more, the article points out the value of non-specialty trained nurses, which makes sense: this is a role that often calls for generalism and a working knowledge of primary care.
c) the authors also point out that care management should not be applied 'to patients who are too sick to benefit.' While there is no citation for this particular assertion, the DMCB likewise not only agrees with that, but points out that regular DMCB readers are already long-familiar with the supporting peer review literature. The DMCB recalls numerous instances in which its health plan senior leaders insisted that care management nurses 'do something' about the catastrophically ill patients that had had numerous inpatient stays, required many specialty physician visits and used some very expensive medications. Experienced care management leaders already know that care management is best 'aimed' at patients that are in the sweet middle: not too well that their risk of an exacerbation is low, but not too sick that nothing could be done.
Now, in addition to quoting the oft Googled, widely read, sometimes quoted and always useful if humble DMCB about care management, you can also quote Dr. Bodenheimer and the Journal.
Here's the citation for your copying and pasting pleasure:
*Bodenheimer T, Berry-Millett R: Follow the money - Controlling expenditures by improving care for patients needing costly services. New Engl J Med 2009;361(16):1521-1523
And here's the pdf for printing or forwarding to your colleagues.
a relative accomplishment
I just got back from riding my bike to and from the hospital to have blood work done. It's pretty cold out there (3C or 37.5F), so I was feeling pretty tough - like a real cyclist with frozen fingertips.
When I came to the big hill just before the hospital, I passed a man riding on the sidewalk. "it's pretty steep," he said, as I edged past.
"It is," I laughed. I admit that I was feeling pretty smug.
Then he took the wind out of my sails. "At 85 years old, it keeps getting a little harder."
When we reached the top of the hill, we had to stop at the lights. He kept chatting, while I had to gulp for air before I could respond.
When the lights turned green, he sailed past me, seemingly fully recovered from the climb.
Maybe I need more air in my tires. Yeah, that's it. Or maybe I need to tackle that hill more often.
When I came to the big hill just before the hospital, I passed a man riding on the sidewalk. "it's pretty steep," he said, as I edged past.
"It is," I laughed. I admit that I was feeling pretty smug.
Then he took the wind out of my sails. "At 85 years old, it keeps getting a little harder."
When we reached the top of the hill, we had to stop at the lights. He kept chatting, while I had to gulp for air before I could respond.
When the lights turned green, he sailed past me, seemingly fully recovered from the climb.
Maybe I need more air in my tires. Yeah, that's it. Or maybe I need to tackle that hill more often.
What’s Next? Follow the Money
With the passage of the Senate Finance bill the health care effort now moves to a critical stage with the Senate Majority Leader and the House Speaker now clearly in charge.The more important effort will be Reid’s. Pelosi’s final product will be more predictable (very liberal) but Reid’s will have to be more practical. Every inch Reid moves away from the more moderate Baucus bill will cause
Tuesday, October 13, 2009
The Bush Doctrine of Health Care Reform and One Anecdote About What's Right About Regional Not For Profit Health Insurers
 Oh my. Reading the news and bloggery about the AHIP-sponsored study by PricewaterhouseCoopers, it’d be easy to conclude that the Forces of Dark have finally been confronted by The Angelic Host. Using terms like ‘dishonest,’ threatening,’ ‘ self-serving and ingenuous’ as well as the mother of all invectives (‘tobacco industry!’), it’s become clear to reform supporters that anyone opposed to the health bills before Congress is Satan’s Spawn. It’s almost like an ironic version of the Bush Doctrine that rationalizes preemptive overwhelming attack on any entity that could give aid to evil-doers.
Oh my. Reading the news and bloggery about the AHIP-sponsored study by PricewaterhouseCoopers, it’d be easy to conclude that the Forces of Dark have finally been confronted by The Angelic Host. Using terms like ‘dishonest,’ threatening,’ ‘ self-serving and ingenuous’ as well as the mother of all invectives (‘tobacco industry!’), it’s become clear to reform supporters that anyone opposed to the health bills before Congress is Satan’s Spawn. It’s almost like an ironic version of the Bush Doctrine that rationalizes preemptive overwhelming attack on any entity that could give aid to evil-doers.The Disease Management Care Blog has a different take and thinks the PWC report provides is useful. It thinks there are too many unknowns in reform to confidently predict the future and appreciates the insights from this worst case scenario analysis.
It’s too bad that the entire health insurance industry is being painted with such a broad brush of loathing. While shrillness makes for good website traffic, it can make the rest of us lose sight of the more subtle issues that are a far better gauge of what’s good about health care in the United States.
Take this local story about the unlucky employees at a company called Turbine Airfoil Designs (TAD), whose company went completely bankrupt months after failing to pay their workers’ health insurance premiums to Capital Blue Cross Blue Shield (CapBSBS). No one outside the leadership of the company apparently knew about the lapse and a number of the workers and their family members, assuming they had insurance, generated some significant health care bills. It was after they got the bad news about being unemployed that they also found that their health insurance hadn’t been in place and they were personally liable. What’s more, some tone deaf hospitals billed their full rate for services (instead of the discounted Cap BCBS rate they had agreed to accept in the first place) and. to add insult to injury, some patients were referred to collection agencies.
What developed what a circle of mutual non-culpability. Thanks to the bankruptcy, the outstanding health care debts got in line with the rest of the company’s creditors. CapBCBS couldn’t have been expected to notify these patients that they didn’t have insurance and arguably shouldn’t use their paying customers’ premium dollars to pay for nonpaying customers. The hospitals argued that they can’t afford to give services away for free. And some proud working class Americans unsurprisingly refused to turn to charity.
So what happened? The Chief Executive Officer of CapBCBS announced that it was going to fix the problem. The rationale that used was:
'Capital BlueCross is a business -- but we also are a nonprofit organization with a 70-year community mission. And this is one of those instances where mission should prevail.'
First of all, The DMCB says bravo to CapBCBS. But don’t be too surprised, because countless regional not-for-profit insurance companies with a local sense of mission and community mindedness would have done the same thing.
Secondly, it doubts very much that the close-minded Forces of Light described above will pay this anecdote any heed.
around the table and around the world
Boy, am I dopey today.
We had our Thanksgiving dinner last night - turkey, mashed potatoes and stuffing (probably the best I have ever had) smothered in gravy. A beautiful salad with a basil and feta dressing. Lots of wine. And Guinness chocolate cake, pumpkin pie, whipped cream, ice cream and chocolate sauce for dessert (I don't think anybody actually had all of those things).
And a truly lovely group of people.
It was perfect.
Today, I am trying to make notes for a presentation I am giving on Thursday. I need to talk about my transformation from individual cancer patient to a member of a vibrant and supportive community.
I had lots of thoughts about this on the week end, when I really didn't have time to write them down. Today, my brain seems to have been replaced with mashed potatoes and gravy (Mmm. Leftovers).
It's an interesting question, though. My online community (which consists of folks I have met in real life and others I probably will only ever know online) has been a key source of information and support over the years.
So, help me out here. What role does your online community play in your life? How did you come to build these virtual relationships? Does the internet help sustain relationships with friends?
I'm not asking you to do my work for me (really, I swear). I'm just curious how you react to the words "network" and "community" and how they apply to your online life.
Labels:
Breast Cancer,
cancer blog,
community,
family,
good stuff,
joy,
kids,
my friends,
my kids,
my love,
thinking
Subscribe to:
Comments (Atom)
