Showing posts with label Medicare. Show all posts
Showing posts with label Medicare. Show all posts
Wednesday, May 25, 2011
Earth to Republicans: You Are In Big Political Trouble Over the Ryan Medicare Plan
It should now be clear to Republicans they are in trouble over the Ryan Medicare plan.Yesterday, they lost a seat in a solid Republican New York House district. Their candidate had benefited from lots of money and House leadership attention. The big issue was the Ryan Medicare plan.All month, Republican Presidential candidates have been walking a tightrope over the Ryan plan--don't embrace it but
Friday, May 13, 2011
The Medicare Patient Empowerment Act (MPAE)
 While the Ryan Plan has insurance vouchers, how about payment vouchers? That's how the Disease Management Care Blog thinks about the Medicare Patient Empowerment Act (MPAE).
While the Ryan Plan has insurance vouchers, how about payment vouchers? That's how the Disease Management Care Blog thinks about the Medicare Patient Empowerment Act (MPAE).Right now, doctors that "participate" in Medicare must take "assignment" for all patients and accept its payment in full and not balance bill. There is a good discussion of how it all works here. The two page MPEA would change that, allowing docs and patients to directly "contract" for service costs over and beyond the Medicare rates, while the physician could still be reimbursed for the amount amount that Medicare would have otherwise paid. The proposed legislation requires that the arrangement be spelled out in a formal written contract and protects the patient from being billed for additional payments that are explicitly spelled out in the contract. The patient would have to agree to things ahead of time and presumably be fully apprised of the out of pocket costs. It also can't be implemented during emergent or urgent care.
The AMA and other MPAE supporters argue that being able to bill for the "balance" of unpaid costs would make it more likely that physicians will continue to see Medicare beneficiaries and "preserve" patient choice. Opponents point out that the threat of drop-outs is a paper tiger and that balance billing will introduce a two-tier system of haves and have-nots, since patients who are unable to 'contract" could be shut out.
Whatever its merits, the likelihood that this will ever get past the Senate and to the President's desk is about as high as the DMCB getting an apology from Google for wiping out some of its recent posts. This is simply another wrinkle in the politically stunted debate over Medicare as a defined "contribution" versus the status quo of a defined "benefit" and it ain't going anywhere. What better evidence of that than this peer reviewed medical evidence that the Republicans have no stomach for the topic.
Thanks to Google blogger being down, the DMCB was unable to post this as originally planned on the curiously ironic date of Friday, May 13. The DMCB apologizes for the inconvenience.
Thursday, April 14, 2011
The Budget Fight: It Will Be A Long Hot Summer, and Fall, and Winter…
The good news is that Democrats and Republicans are finally seriously engaged over the country’s fiscal crisis.And, each side is presenting a starkly different course for the voters to choose from.When it comes to the health care entitlements, Republicans want to cut the health care entitlement benefits and therefore ease the pressure on federal spending.Obama wants to largely leave the programs
Tuesday, November 23, 2010
Will it Be the Bond Market That Finally Forces Serious Health Care Financing Change?
When will the Congress and the White House finally make the hard decisions in order come to grips with the federal deficit problem?When will we finally deal with real health care reform and get the entitlements, and with them the private health care cost issue, under control?My focus on trying to answer those questions has always centered on what's going on in the health insurance market: When
Thursday, November 11, 2010
Shame on AARP For Their Response to the Deficit Commission Co-Chairs' Report
The Co-Chairs of the President’s Deficit Reduction Commission are out with their preliminary recommendations.They’ve done a great job—they’ve offended about everyone!But we have a nearly impossible but unsustainable challenge in front of us if we are ever going to crawl out of this deep hole.It is not so much what is on their list as what this list tells us about just how fundamental the changes
Thursday, October 28, 2010
Open the Medicare Claims Data Base to the Wisdom of Crowds.
 If you believe that CMS has what it takes to make sure that Medicare claims are paid the right way for the right patients most of the time, you may need to think again. According to this article in the Wall Street Journal, it's too easy for the government to misspend millions of dollars for dubious care involving questionable doctors.
If you believe that CMS has what it takes to make sure that Medicare claims are paid the right way for the right patients most of the time, you may need to think again. According to this article in the Wall Street Journal, it's too easy for the government to misspend millions of dollars for dubious care involving questionable doctors.But Medicare's fiduciary ineptness is not why this article is worth reading.
If you believe the Journal, the Medicare claims data base, otherwise known as the "Carrier Standard Analytic File" is a gold mine of information that, but for archaic privacy laws, could be used to spot those questionable doctors. Organized physician groups have generally opposed the public release of those doctors' names, even if it involves public money.
But physicians' right to privacy vs. the public interest is not why this article is worth reading.
Rather, this article is important because it portrays the power of allowing open access to the government's health insurance claims databases. The Journal simply sorted Medicare claims costs by provider and came up with some potentially important insights. Imagine, says the DMCB, what would happen if everyone could access the data from the world's largest insurer and mine it for correlations, regressions and other statistical whattnot. There are a host of amateur statisticians who could not only uncover important practice patterns, but mine other unknown associations involving demographic information, the incidence of disease and likelihood of successful cure. It's called the wisdom of crowds.
While privacy for patients and physicians is important, reasonable protections are possible. As for Medicare itself, the program would not only benefit from the clinical insights that would be uncovered, but other investigations similar to the Journal's might make it more responsive to acting on potential fraud.
Last but not least, those data belong to the American public.
The data are too useful to lock away from its owners. This is an idea whose time has come.
Wednesday, July 21, 2010
Getting All Americans Covered Falls By The Wayside
 The Disease Management Care Blog gained one major insight during its recent Washington DC health care conference.
The Disease Management Care Blog gained one major insight during its recent Washington DC health care conference.In all the talk about "health reform," there was very little discussion about one of the past leading justifications of the Affordable Care Act (ACA): that by giving tens of millions of Americans insurance, there'd be more preventive and screening services, earlier care for chronic illnesses and better access to hospitals after unexpected illness. It was argued that disease detection would be increased, and disease progression would be decreased and avoidable high-cost complications would be... well... avoided. The expensive and shameful "hidden tax" of unnecessary and inefficient cost-shifting would be replaced by enlightened and cost-effective public financing.
There may be merit of the argument, but it's conspicuous absence at a D.C. conference and, by the way, in many of the health journals, policy media and blogs makes the DMCB think that many of the cognoscenti silently doubt it. Ask policymakers and academics about bending the cost curve today and what you'll get is a refrain consisting of bundled payments (that intelligently capitate physician services), primary care medical homes (that shift health services to a cheaper level of care) and accountable care organizations (that align all the economic incentives).
The DMCB sees the merits of each of those concepts. Congress obviously did also when it mandated them in a variety of demos and pilot programs. What's more, the ACA is remarkable for the power it gives to the HHS Secretary to rapidly expand them, and to do so without Congressional approval.
Which is the rub. While the Secretary's flexibility is a good thing, the one thing that is standing in her (or his) way is that the pilots/demos really have to show cost savings. While many of my colleagues believe that is a mere formality, the DMCB recalls many in the disease management industry felt the same way about Medicare Health Support Demo. It didn't quite work out as planned.
Which brings the DMCB to the ultimate question: if the pilots and demos don't work, just what is "Plan B?" The answer at the Conference, for Medicare at least, was across the board delays in any scheduled fee schedule increases and/or reductions. Yikes.
Which is the insight. The discussions about the possibility of across-the-board cuts may have greater visibility today than merits of extending insurance to the uninsured. It's not out there in the media. so you read it here first.
The DMCB will continue to monitor this.
Tuesday, July 20, 2010
The Limits of a "Successionist" Mind Set in the Search for Payment Innovation in Medicare
 The Disease Management Care Blog survived today's panel discussion at the 6th Annual Leadership Summit on Medicare. We discussed CMS' search for payment innovation that leads to increased quality with lower costs.
The Disease Management Care Blog survived today's panel discussion at the 6th Annual Leadership Summit on Medicare. We discussed CMS' search for payment innovation that leads to increased quality with lower costs.The DMCB started out by noting that not all quality means lower claims expense. What's more, even if there are savings, the cost of delivering the quality can negate any savings. There are ways around that, but that's for another post. Something far more interesting came up.
The DMCB focused on the more fundamental issue of measurement methodology. If you think about it, this typically uses a "successionist" mind set. In other words, scientists and policymakers expect that if an intervention is made in a system and everything else is held neutral, that anything that follows must have been "caused" by the intervention. Succession means "the act or process of following in order or sequence." The study of interventions and how they lead to outcomes forms the basis of health services research, evidence-based medicine, clinical research trials and the like.
There are two problems with using the successionist mind set to assess the quality and costs that follow medical interventions:
1) The measurement environment is statistically "noisy," including a general upward trend in overall health care costs. Picking out the impact of a single intervention is like trying to hear the East River's tug boats from atop of New York City's Empire State Building.
2) Health care is a messy, complex social system with many moving parts. It's hard to control the other factors that play a role in quality and cost, especially from a patient's point of view. That makes it hard to know just what caused the movement of those tug boats.
There are solutions though. The DMCB paraphrases from an excellent article that appeared in JAMA back in 2008:
A successionist tool kit that holds all sources of bias neutral while [what] it measures ... may be unequal to the task of evaluating complex, nonlinear, interpersonal social programs, with findings that ... [are] ... typically non-cumulative, low-impact [and] prone-to-equivocation. The emphasis on knowing whether something works leads to little insight on how/why it works. There are four ways to overcome this:
1. Use a wider range of research methodologies that draw on ethnography, anthropology and other qualitative methods.
2. Reconsider the threshold for action on evidence, especially if the status quo is unacceptable.
3. Measure bias, don’t seek to eliminate it. The knowledge of trusted insiders may be more powerful than the conclusions of distant third party evaluators.
4. Don’t get in the way with insistence on weighing evidence with impoverished tools but asking what is everyone learning.
The DMCB agrees that CMS needs to think about incorporating these approaches in its search for value.
Who wrote this, you ask? Don Berwick, the new Administrator at CMS. The link is here.
Thursday, July 8, 2010
The Risk of a Physician Boycott of Medicare, Congress' Duty, Enterprise Risk Management & What MedPAC Should Do
 The Disease Management Care Blog thinks of Medicare as a large health insurance company overseen by a Board of Directors that just also happens to be called "Congress." As a Board, Congress' job is to provide oversight, including approving the benefit, premium levels and the provider fee schedules. Like other Boards, it's also supposed to be ultimately responsible for the appointment of executive leadership. Last but not least, it should engage in "enterprise risk management" (ERM). More on this later.
The Disease Management Care Blog thinks of Medicare as a large health insurance company overseen by a Board of Directors that just also happens to be called "Congress." As a Board, Congress' job is to provide oversight, including approving the benefit, premium levels and the provider fee schedules. Like other Boards, it's also supposed to be ultimately responsible for the appointment of executive leadership. Last but not least, it should engage in "enterprise risk management" (ERM). More on this later.Medicare's "Board" has struggled with the cumulative costs of repeatedly delaying the Sustainable Growth Rate (SGR) reductions for the Part B fee schedule. A perfect storm of election year politics, deficit spending concerns and partisan brinkmanship has led to another "temporary fix" of the scheduled 21% cut. The day of reckoning has been pushed back to November 30, 2010. While grumpy organized physician organizations are publicly concerned about the SGR's impact on patient "access" and "choice," the real threat is that many physicians who currently accept Medicare will "go Texan" and boycott the Medicare if the SGR goes through.
Should Medicare's "Board" be concerned?
As the American College of Physician's* (ACP) Advocate Blog's Bob Doherty points out, physicians have been repeatedly warning for years that Medicare's payment rates are unsatisfactory. In the meantime, the Medicare Payment Advisory Commission (MedPAC), which uses surveys of Medicare beneficiaries to gauge whether physicians really really mean it, remains unmoved. According to MedPAC's data, the vast majority of Medicare beneficiaries still have adequate access and most docs still accept Medicare. Liberal pundits, such as Maggie Mahar, think that threat of a physician boycott is an "overblown" paper tiger unsupported by facts on the ground involving real docs, like hospitalists, cardiologists and geriatricians.
Yet, the ACP's Bob Doherty wonders if things could be different this time. His anecdotal conversations with docs makes him think that substantial - if unquantifiable - numbers of physicians are really thinking about dropping out of Medicare.
Which brings the DMCB back to the topic of "ERM." This is defined as the systematic and objective quantification of all significant risks to a business. ERM typically includes identifying what risks exist, their individual likelihood, their potential magnitude, strategies for their mitigation and assessing progress in keeping them at bay.
Congress' Medicare ERM issues are multiple and include the growing number of baby boomer beneficiaries, their considerable appetite for pricey technology, looming government debt and the involvement of sophisticated organized crime networks in Medicare fraud. But one important risk that continues to languish is the SGR and the potential for a physician backlash.
The DMCB thinks Medicare's Board, i.e., Congress should perform its fiduciary duty and use ERM to carefully examine the issues raised by Mr. Doherty.
What is the risk of a physician boycott?
While the prospect of a wholesale nationwide exodus of physicians from Medicare participation is still small, it is not zero and, given Mr. Doherty's credible suspicions, the risk is growing. The risk is probably greater among the smaller physician owned practices with access to alternate sources of patient care income. It's likely to first show up in refusals to accept new Medicare patients. It'll occur regionally (Texas may be a good example) and vary by practice specialty. The risk is highest among the "cognitive" physicians who a) can't make up for lost revenue with additional patient volume, and b) are dealing with payment rates that have been widely regarded as inadequate.
What is the potential magnitude?
There are two dimensions: operational and political.
It's operationally moderate because of two factors:
1) the relationship between the threat of an SGR reduction and a physician boycott is not linear. While current physician Medicare non-participation rates are low, reaction to inadequate payment rates could quickly cascade under a classic self-reinforcing phenomenon. This is discussed by the DMCB in greater detail here,
and
2) the interplay between spotty regional access issues and other parts of the health care system - even if access is maintained - could lead to further stressors. While low numbers of Medicare beneficiaries per primary site may not be able to receive primary care, the phenomenon at a regional level across multiple sites could easily lead to delays in care, emergency room crowding and spikes in avoidable hospitalizations.
It's politically high because even spotty regional access problems could be spotlighted by the news media and used by opponents of health care reform to further gum up the President's agenda.
How can it be mitigated?
It's going to take either a) finding new money or b) moving money from other sources. That's the topic for another DMCB post but two additional points should be made:
1) thinking that "savings" from efficiencies, prevention, wellness or the electronic medical record, medical home and accountable care organizations demos and pilots will solve the SGR is fanciful thinking. Don't even bring it up, because the doctor-audience won't believe you. They're too smart.
2) Just the threat - real or not - of an SGR reduction is undoubtedly causing physicians to plan for the possibility of a boycott. Accordingly, "the SGR" needs to be removed from the public spotlight and replaced by a credible signal that Congress and the Administration are taking Medicare payment rates seriously.
How should progress be measured?
In addition to regularly reading the ACP and DMCB blogs (and being skeptical about the can-do-no-wrong loyalty of liberal media sycophants), MedPAC should reinvigorate its reports (like this one that said no problem) and reexamine access from the perspective of ERM with special attention to specialty, region, practice size, non-linearity and worse case scenarios.
The Federal government failed to adequately assess the environmental risks of deep water oil drilling and the systemic financial risks from the easy money and housing bubble. It's not unreasonable to ask if MedPAC is on the verge of committing the same mistake in a key part of healthcare policy.
(Addendum: Interested in this debate? There's more here)
*an organized physician group that represents internists, who focus on prevention, diagnosis, and treatment of adult diseases. The DMCB not only a proud member of the AMA, it is an internist and an ACP Fellow.
Wednesday, July 7, 2010
Don Berwick Becomes Part of the Problem
 According to the New York Times, a "recess appointment" will be used to install Don Berwick as the CMS Administrator. It seems this was the only way the Obama Administration could bypass those obstreperous Senate Republicans, who were apparently planning to abuse the confirmation process with toxic puffery, "gotcha" politics and other forms of unpleasantness.
According to the New York Times, a "recess appointment" will be used to install Don Berwick as the CMS Administrator. It seems this was the only way the Obama Administration could bypass those obstreperous Senate Republicans, who were apparently planning to abuse the confirmation process with toxic puffery, "gotcha" politics and other forms of unpleasantness.There are plenty of good arguments in favor of the recess appointment, including fixing an obvious leadership vacuum at the worlds largest health insurer, accessing Dr. Berwick's considerable skills in implementing countless details of the Affordable Care Act (ACA) and capitalizing on his widespread support from the multiple corners of the health care industry. As my liberal colleagues like to point out here and here, this is also an opportunity for the Administration put its reasonable centrism on display while reminding its base of its commitment to health reform and simultaneously poking the eye of a bullying opposition.
While the non-liberal contrarian Disease Management Care Blog was among the first to endorse Dr. Berwick, it respectfully if naively disagrees with the strategy of a recess appointment. Here's why:
1. The Body Politic: While he's well known among physician and policy types, this was an opportunity to use a visible forum to introduce Dr. Berwick to other constituencies less familiar with him and his important ideas. Our nation's healthcare dialog did not end with the passage of ACA.
2. Transparency: Dr. Berwick's academic record, obvious leadership record and considerable rhetorical skills are more than a match for the Senate's scrutiny. Who is afraid of who?
3. Seizing the High Road (OK, it is the oxymoron of politics, but....): Republicans threatening to behave badly and remind Americans about their dysfunctions is a problem for the Democrats? In the few months until the election, it may be time for the Dems to start rolling the dice on acting honorably.
4. It stinks! Speaking of dysfunction, is the outcome of expediency worth short circuiting merits of a Senate supermajority? Will Dr. Berwick's credibility over the next two years be hampered by the recess appoointment? The Obama Administration is one-upping the opposition's political maneuvering with their own. The whole thing brings discredit to both parties.
5. Bloggery: The confirmation hearings promised to be a cornucopia of detailed analysis, second guessing and extreme wonkism. Darn.
Of course, even the DMCB isn't too sure that, if it were Dr. Berwick, it would have been able to resist the sure bet of a recess appointment in lieu of bruising Senate confirmation. There's something to be said, however, for the selfless heroism of the third option: respectfully declining the CMS post with the option of reconsidering when one of three things happen: 1) both sides get serious about putting the people's business over politics or 2) the bums get replaced by politicians who know how to compromise or 3) the Feds realize that intelligently centrally controlling health care is a myth.
Unfortunately, accepting the recess appointment continues business as usual.
As for things changing, the DMCB isn't holding its breath.
Coda: It didn't occur to the DMCB that the confirmation process posed election risks for some incumbent Democratic Senators. One small consolation is that at least Senator Baucus (D-MT) understands the bigger picture.
Thursday, June 10, 2010
CMS Steps Up With the Multi-Payer Advanced Primary Care Practice Demonstration on the Patient Centered Medical Home (PCMH) at $10 PMPM
 Readers have questioned the Disease Management Care Blog about its Facebook and the other glow-pink eyed portraits in the right side of the page. It's been told that it conveys a buffoonishness that is inconsistent with the DMCB reputation of sober erudition and morose skepticism. What's more, it's been asked: just what are those lights?
Readers have questioned the Disease Management Care Blog about its Facebook and the other glow-pink eyed portraits in the right side of the page. It's been told that it conveys a buffoonishness that is inconsistent with the DMCB reputation of sober erudition and morose skepticism. What's more, it's been asked: just what are those lights?Well, the pic is not long for this blog, but that doesn't mean it doesn't hold a special place in the DMCB Galaxy. Those are, by the way, pink flamingo tree lights, surreptitiously added to the cart by DMCB after being invited by the spouse to accompany her on a holiday shopping errand months ago. Despite the DMCB's merry participation, it was pointedly warned during check-out that this was the "last time" it would "ever" etc. etc. It seems it turned left in the aisles when it was supposed to go right, touched things it shouldn't have and said things that weren't helpful. While the lights were disappointingly never tasked to their original celebratory purpose, the DMCB has discovered - despite occasional attempts at spousal sabotage - that they are suitable for year-round display in the Executive Suite of DMCB World Headquarters.
And the States with Patient Centered Medical Home (PCMH) pilots may gain a special appreciation for the DMCB spouse's travails after they're done checking out just how CMS intends to merrily participate in their programs. The Feds have just released their "solicitation" for their "Multi-payer Advance Primary Care Practice Demonstration." This is **THE** three year demo designed to test the PCMH across multiple insurers, including Medicare fee-for-service (FFS).
Recall that one big problem encountered by the current bevy of pilots is that they're typically sponsored by just one or a few insurers. As a result, it's been difficult to ask primary care practices to reengineer their daily workflows to offer the "Cadillac" PCMH to patients with one type of insurance and "Chevy" usual care to patients with another type of insurance. Up until now, Medicare has relegated its patients to the Chevy.
Can the Cadillac PCMH pay off in Medicare FFS? To find out, CMS is inviting up to six States with ongoing multi-payer pilots to submit applications by August 3, 2010.
CMS' requirements are considerable. It wants (in "40 pages or less"):
1) a State agency to lead it,
2) enlistment of multiple group/individual private payers (that together enroll ">50% of State residents") as well as its Medicaid program,
3) the State to"demonstrate [the] commitment" of majority of its PCPs,
4) identification of and a way to certify PCMHs that also have links to State/community, public health, wellness and prevention resources,
5) to have the provider payment mechanisms in place,
6) CMS's uniform payments for the clinics/coordination/CMS' share of the administrative expenses (plus not to exceed $10 PMPM) all set up,
7) a way to figure out how to "attribute" a beneficiary to a PCMH (for example, by "designation"),
8) the State to line up any necessary waivers,
9) the creation of an adequate monitoring system,
10) State agreement to participate in an independent evaluation by an entity of CMS's choosing,
11) a reasonable assurance that the demo will be "revenue neutral" ("describe the anticipated effect of the State initiative on aggregate or global expenditures under the Medicare program for all covered services combined"), and
12) be ready to go by the end of 2010.
The DMCB's first reaction is that these requirements to the States and their physicians will be, er.... daunting. It is going through the other documents on the CMS web site and will be pondering them over the appropriate beverages this weekend. Look for lots more on the topic here.
Tuesday, February 9, 2010
Ms. Sebelius and Wellpoint's Rate Increases: Doesn't HHS Have Enough to Worry About?
 Egads, doesn't Ms. Sebelius have enough to worry about?
Egads, doesn't Ms. Sebelius have enough to worry about?Our HHS Secretary faxed a letter to California-based Anthem Blue Cross, expressing how 'disturbed' she was by 'unaffordable' rate increases 'as much as 39%' in the face of 'soar'ing $2.7 billion profits. She calls for greater transparency on the ratio of medical vs. overhead costs and urges Anthem to 'cooperate fully' with California's Insurance Commissioner, because [gulp!] she will be 'closely monitoring the situation.'
While the Disease Management Care Blog appreciates this latest example of perma-campaign mode political grandstanding, it would like to remind the HHS leadership that there is no national health insurance comissioner with jurisdication over state regulated plans. Ms. Sebelius' considerable administrative and political skills would be better spent addressing the government's 10.4% trend rate, relentless growth to the point of accounting for 50% of all health care costs, a budget increase in 2011 in excess of $80 million with close to 3000 additional FTEs, not having anyone at the helm at CMS, and a looming deficit that has perilous national security implications.
The DMCB hopes that Ms. Sebelius' puffery wasn't completely orchestrated by the White House's Four Horsmen and that she actually took the took the time to personally look at Wellpoint's 2009 financials. If she did, she'd know the company lost 1.4 milion members, mostly from its small group business. Operating revenue went down compared to 2008, the cost trend was high at 8.9% thanks to rising provider costs and investment income was lower. The DMCB suspects it all adds up to a toxic brew of premium increases due to a combination of higher medical costs and unfavorable underwriting: in the current economy, healthy persons that can do without insurance drop it, leaving behind relatively more sick persons with high health care costs. The DMCB wonders why no one has pointed out that a rate increase was the responsible thing to do in the face of relentless health system cost increases - unless, of course, you're willing to trample on State's rights, fudge entitlements, print money and borrow from the Chinese.
Ms. Sebelius can fuss all she wants. The there are only so many premium dollars to cover the cost, the State of California is in charge, and the Obama Administration's time would be better spent on dealing with bigger problems that it can actually do something about.
Current and future Medicare beneficiaries deserve better.
++++++++
Addendum:
For an update on how things can snowball (no pun intended for those of us living in the Mid-Atlantic), check out the investigative spleen venting in the Health Access WeBlog. The veteran Bob Laszewski has more middle-of-the-road perspective here at the Health Care Policy and Marketplace Review Blog.
The DMCB is going to double down and predict that, once the news cycle moves on, Anthem will quietly provide all its pricing information to all the various Committee Chairs, Senators, Commissioners, Commissars and Potentates. After a requisite amount of nit-picking and face-saving adjustments, the bulk of the premium increases will stand. That's because, in this particular instance, health care inflation and the political process are the real problems, not the health insurance industry.
Wednesday, February 3, 2010
The Tea Baggers Just May Have a Point About Health Care.....
 Back in the 1960s, the Twilight Zone regaled television viewers with fantastic stories from a place between 'science and superstition,' that lay 'between the pit of man's fears and the summit of his knowledge.' Approximately thirty years later, popular culture was introduced to an even more surreal place in the 1979 film The Black Hole. Disney's state-of-the-art special effects portrayed a space environment dominated by a distant, visually compelling and vaguely sinister hyper-gravitational spinning black hole. As testimony to their commercial success, the terms 'twilight zone' and 'black hole' remain instantaneously recognizable today, describing situations where the usual laws of gravity, time and common sense are unpredictably and variably suspended.
Back in the 1960s, the Twilight Zone regaled television viewers with fantastic stories from a place between 'science and superstition,' that lay 'between the pit of man's fears and the summit of his knowledge.' Approximately thirty years later, popular culture was introduced to an even more surreal place in the 1979 film The Black Hole. Disney's state-of-the-art special effects portrayed a space environment dominated by a distant, visually compelling and vaguely sinister hyper-gravitational spinning black hole. As testimony to their commercial success, the terms 'twilight zone' and 'black hole' remain instantaneously recognizable today, describing situations where the usual laws of gravity, time and common sense are unpredictably and variably suspended.Since thirty years have passed, it may be time to recognize another fantastical environment, described in this Health Affairs web exclusive, titled 'Prices Don’t Drive Regional Medicare Spending Variations,' by Daniel Gottlieb, Weiping Zhou, Yunjie Song, Kathryn Gilman Andrews, Jonathan Skinner and Jason M. Sutherland.
Basically, the authors examined critical three factors in the regional variation of Medicare's per capita health spending: 1) the additional money allocated for teaching hospitals, 2) the additional money allocated for the care of the socioeconomically disadvantaged and 3) local differences in the cost of living, which influences pricing of medical services. The bottom line is that when these elements are mathematically 'backed out,' per capita variation in health care spending is only dampened sightly and is still all over the board.
How can this be?
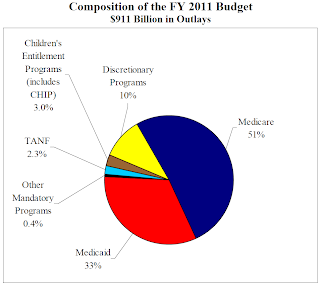
While it's still up to readers to decide if some of the variation can be explained by local poverty and its effect on hospital quality, the Disease Management Care Blog is still struck by Medicare's surreal distortion of the time-space fabric of the health care market universe and how easily the viewer can be sucked into this logic-defying time-space of contractors, DRGs, RVUs, ineffective cost controls, inefficient mainframe-style central planning, political zg zagging, cumbersome denials, attacking the inevitable outliers, provider gaming and a sprawling $911 billion bureaucracy.
There is plenty of blame to go around for this dysfunction and, let's face it, Medicare and Medicaid have led to unparalleled health benefits for the poor and elderly. Yet, persons looking into the distorted market of two to threefold cost differentials with no discernible impact on quality must be puzzled by how the black hole can bend a line of reasoning toward greater government involvement.
The DMCB not suggesting the CMS be cancelled, any more than it can cancel black holes: both are embedded in our time-space continuum.
But it also cautions against tut-tutting those wacky cranky Tea Baggers and their common sense look at 'government style health care.' The cognitive dissonance of 'getting government out of Medicare' belies a deeper reality: once you step outside the Twilight Zone and away from the Black Hole, it's pretty obvious that government's management of the program is not of this earth.
Tuesday, January 26, 2010
The State of the Union, Health Reform and the Need for a CMS Administrator: The Time is Now
 No doubt, at the time of this posting, the President and his aides are huddling over the upcoming State of the Union Address. Barring any more outbursts from the now emboldened Republican members of Congress, the Disease Management Care Blog thinks one of the more dramatic moments of the speech will be the unveiling of Mr. Obama’s reconfigured health policies. Will he go for broke and push for passage of an unchanged Senate bill? Will he go opaque with vague bromides about access and quality? Will he go on a populist anti-insurer bender and announce that there’s a new sheriff in town? Will he grin, turn and high-five with Ms. Pelosi and declare the dream will never die? Will he offer a bipartisan man-hug to the Republicans?
No doubt, at the time of this posting, the President and his aides are huddling over the upcoming State of the Union Address. Barring any more outbursts from the now emboldened Republican members of Congress, the Disease Management Care Blog thinks one of the more dramatic moments of the speech will be the unveiling of Mr. Obama’s reconfigured health policies. Will he go for broke and push for passage of an unchanged Senate bill? Will he go opaque with vague bromides about access and quality? Will he go on a populist anti-insurer bender and announce that there’s a new sheriff in town? Will he grin, turn and high-five with Ms. Pelosi and declare the dream will never die? Will he offer a bipartisan man-hug to the Republicans?Stay tuned!
And, while all this is going on, there are rumors that an Administrator for the Centers for Medicare and Medicaid Services ('CMS') is about to be nominated.
Finally!
The DMCB appreciates that the folks in the White House may be somewhat distracted with a host of health reform details, but that isn’t going to stop it from giving Team Obama some start-of-the-second-year-of-the-term advice:
It's been too long. It's time to get a duly empowered Administrator to lead the Department of Medicare and Medicaid Services.
While the current Acting Administrator is certainly qualified, let’s face it: if CMS is truly going to be an active partner-participant in state and national efforts at health reform, it needs a leader that not only passes muster with Congress but with the American people. The optimistic DMCB also thinks that the confirmation process could - emphasis on could - be an important opportunity to kick-start a stalled bipartisan dialog on health reform.
What’s more, it appears to the DMCB that, up until now, the White House’s health policies have been largely represented by the very intelligent but, let’s face it, lawyerly bureaucrat, Ms. Nancy DeParle. While she certainly has her capable hands full outside of the public eye, it's been too easy for those of us outside of the beltway to conclude that the President's health reform efforts have gone from disengaged to rudderless. What's more, CMS has been curiously lacking in innovation, flexibility and leadership. Case in point? The Lifemasters fiasco. There has never been a greater need for the Agency to adopt a broadminded approach to modern population-based care management than now.
And, while all this is going on, there are rumors that an Administrator for the Centers for Medicare and Medicaid Services ('CMS') is about to be nominated.
Finally!
The DMCB appreciates that the folks in the White House may be somewhat distracted with a host of health reform details, but that isn’t going to stop it from giving Team Obama some start-of-the-second-year-of-the-term advice:
It's been too long. It's time to get a duly empowered Administrator to lead the Department of Medicare and Medicaid Services.
While the current Acting Administrator is certainly qualified, let’s face it: if CMS is truly going to be an active partner-participant in state and national efforts at health reform, it needs a leader that not only passes muster with Congress but with the American people. The optimistic DMCB also thinks that the confirmation process could - emphasis on could - be an important opportunity to kick-start a stalled bipartisan dialog on health reform.
What’s more, it appears to the DMCB that, up until now, the White House’s health policies have been largely represented by the very intelligent but, let’s face it, lawyerly bureaucrat, Ms. Nancy DeParle. While she certainly has her capable hands full outside of the public eye, it's been too easy for those of us outside of the beltway to conclude that the President's health reform efforts have gone from disengaged to rudderless. What's more, CMS has been curiously lacking in innovation, flexibility and leadership. Case in point? The Lifemasters fiasco. There has never been a greater need for the Agency to adopt a broadminded approach to modern population-based care management than now.
Here's to a CMS Administrator nomination that showcases a commitment to meaningful health reform and the return of a CMS that is a credit to the American people.
Monday, October 12, 2009
The Transmogrifying of Fee-For-Service Medicare into Managed Care
In one episode of the long retired comic strip Calvin and Hobbes, the highly imaginative and socially dysfunctional Calvin invents the Transmogrifier. The answer to all both large and small boys’ fondest wishes, this upside down cardboard box is controlled by a large dial that can change its passenger into any shape. Its settings include tiger, bug, eel and dinosaur. The Disease Management Care Blog would really like to have one of those and include ‘motorcycle owner’ on the dial, but, alas, the DMCB spouse will have none of it.
Outside of the DMCB's imagination, however, a very real version of the Transmogrifier lives on thanks to the Congressional plans for Medicare. How else can Medicare dial in ‘value based purchasing,’ ‘quality and efficiency,’ ‘accountability,’ and taxpayer savings’ without the use of an imaginary cardboard box and even more imaginary money?
Armed with these key insights about just what defines managed care, DMCB compared some key features of the U.S. Senate Finance Committee’s Framework to see if ‘managed care’ belongs on the dial. It may:
Selective Contracting: Under value based purchasing, only hospitals that meet yet-to-be-determined quality thresholds will receive favorable payment rates..
Predetermined Monthly Premiums: While unmentioned in the Framework, the payment mechanism for patients assigned to Medical Home pilots is likely to be a monthly fee. This is otherwise known as partial capitation, which is a common approach in managed care networks.
Utilization and Quality Controls: Physicians that exceed, compared to their peers, ordering high cost imaging services will be penalized. The only difference here is that physicians won’t have much of an opportunity to not agree.
Financial Incentives: That ‘I’ word is used to encourage Medicare beneficiaries to participate in healthy lifestyle programs that meet yet to be determined criteria.
Financial Risk: Under accountable care organizations, providers would be able to keep half of any savings they achieve for the Medicare program. While there are safeguards to promote quality, the fact is that the physicians will be under pressure to balance the patient’s needs against the need for cost control.
In the meantime, the DMCB plots its nefarious revenge on its wannabe Susan Derkins DMCB spouse.
Outside of the DMCB's imagination, however, a very real version of the Transmogrifier lives on thanks to the Congressional plans for Medicare. How else can Medicare dial in ‘value based purchasing,’ ‘quality and efficiency,’ ‘accountability,’ and taxpayer savings’ without the use of an imaginary cardboard box and even more imaginary money?
Yet, our imaginative and dysfunctional legislators have left one key setting off of the dial, and that’s ‘managed care.’ They should put it on because that's exactly what the Transmogrifier is going to accomplish for Medicare when they get done.
Here's why.
Other than Medicare Advantage, most versions of Medicare so beloved by the Democrats and many of our seniors is a fee-for-service indemnity plan. This means it insures the beneficiary against a financial debt (or 'indemnity') incurred as a result of medical treatment for an illness. While Medicare has the advantage of fee setting, its role in the clinical decision-making in the doctor-patient relationship has been historically quite small.
Contrast the coming legislative proposals for Medicare with managed care insurance. According to this link, 'managed care' is any health insurance that uses of a variety of methods of financing and organizing the delivery of health care in which an attempt is made to control costs by controlling the provision of services. These methods (according to this link) can include 1) contracting with selected physicians and hospitals usually for a predetermined monthly premium 2) utilization and quality controls that contracting providers agree to accept, 3) financial incentives for patients to use the provider and facilities associated with the plan and 4) the assumption of some financial risk by doctors, thus fundamentally altering their role from serving as agent for the patient's welfare to balancing the patient's needs against the need for cost control.
Armed with these key insights about just what defines managed care, DMCB compared some key features of the U.S. Senate Finance Committee’s Framework to see if ‘managed care’ belongs on the dial. It may:
Selective Contracting: Under value based purchasing, only hospitals that meet yet-to-be-determined quality thresholds will receive favorable payment rates..
Predetermined Monthly Premiums: While unmentioned in the Framework, the payment mechanism for patients assigned to Medical Home pilots is likely to be a monthly fee. This is otherwise known as partial capitation, which is a common approach in managed care networks.
Utilization and Quality Controls: Physicians that exceed, compared to their peers, ordering high cost imaging services will be penalized. The only difference here is that physicians won’t have much of an opportunity to not agree.
Financial Incentives: That ‘I’ word is used to encourage Medicare beneficiaries to participate in healthy lifestyle programs that meet yet to be determined criteria.
Financial Risk: Under accountable care organizations, providers would be able to keep half of any savings they achieve for the Medicare program. While there are safeguards to promote quality, the fact is that the physicians will be under pressure to balance the patient’s needs against the need for cost control.
If it looks like managed care, and if it walks like managed care .....
Finally, while our political elite fault our seniors for their ‘inexcusable’ cognitive dissonance by 'wanting government out of Medicare,' this may be less evidence of flyover state ignorance than an awareness that their passive indemnity insurance is morphing into growing government activism in the doc-patient relationship. It seems to the DMCB that their concerns deserve more than sympathy or disdainful annoyance. This is a real policy direction that deserves closer scrutiny.
In the meantime, the DMCB plots its nefarious revenge on its wannabe Susan Derkins DMCB spouse.
Thursday, August 27, 2009
The Health Reform Bills Would Be Great For the Business Of Health Care
Have you noticed how none of the big health care business special interests is running any negative health care reform ads? Why should they when each is poised to gain billions of dollars from it?As President Barack Obama has said many times, any health care bill that costs about $1 trillion would be paid for, roughly half and half, with savings in the health care system and new revenues (taxes).
Wednesday, August 19, 2009
Medicare: A Mainframe Using Levers. Why Health Reform Is So Complicated
 Drive through Hartford Connecticut on Route I-84 and you cannot miss Aetna's huge corporate headquarters. Or how about visiting Indianapolis and running into Wellpoint’s headquarters? That’s a big impressive building too. The Disease Management Care Blog had seen both of these insurance behemoths, but it can assure you that they’re pipsqueaks compared to what’s at 7500 Security Boulevard in Baltimore.
Drive through Hartford Connecticut on Route I-84 and you cannot miss Aetna's huge corporate headquarters. Or how about visiting Indianapolis and running into Wellpoint’s headquarters? That’s a big impressive building too. The Disease Management Care Blog had seen both of these insurance behemoths, but it can assure you that they’re pipsqueaks compared to what’s at 7500 Security Boulevard in Baltimore.The DMCB recently visited our Centers for Medicare and Medicaid Services and was blown away by the size of the place. The buildings are not only colossal, the parking lot is probably visible from space. Two words occurred to the DMCB on its way out of the complex: mainframe and leverage.
The word mainframe, coined by former HHS Secretary Leavitt, probably doesn’t do it justice, because CMS is obviously far more, well.... organic like the DNA controlled machines in the movie District 9. Armed with a unique combination of information technology and human resources, this nation-state has a budget that exceeds most countries’ GDP. It somehow manages to move hundreds of billions of dollars around in an opaquely complex system of policies, regulations, claims processing and provider billing. It probably uses more processing power and full time equivalents than what was used to put men into space and describe Britney Spears' behavior combined.
It’s the money that also prompted the DMCB to think about one of the earliest and simplest tools known to mankind: the lever. Since CMS is a payer, its administrators understand that economic incentives can be used to incent or disincent the provision of health care services. While CMS’ influence is far more complicated, a bottom line is that its machinery is increasingly being used to manipulate provider and patient behavior.
Why is this important? Aside from the observation that big bureaucracies with imperfect levers seek to become even bigger bureaucracies with more levers:
1. The ability of so vast an enterprise to fine tune its leverage across an even more complicated U.S. health care landscape can be questioned. For example, DRG-based prospective payment reform was successful in decreasing hospital lengths of stay, leading to earlier discharges. The line that separates early from premature discharges is thin, however, especially when good discharge planning is lacking and patients get readmitted. CMS is now piloting paying for the former and increasingly not paying for the latter. Think hospitals won't respond by doing everything they can to not re-admit patients, even if that would be in their best medical interest? Can the mainframe develop a new lever to address this, or will there be even more unintended consequences? How will this work in downtown LA, in Peoria and in Boise?
2. Man lives by more than bread alone. The rich web of relationships that exist between doctors and patients are driven by far more than money, but when all you have is a lever, all the world looks like a moveable object. Leaving aside the conflict of interest in a health insurer trying to promote living wills, the DMCB doubts CMS’ paying for living will counseling will meaningfully increase their use. It’s already easy for physician to ‘bill’ CMS for patient encounters that include such discussions, but it’s not happening. The reasons for this lapse are multiple (and maybe the topic of a future posting) and most are not a function of an undersupply of shekels from CMS.
3. Which leads to the combination of mainframe reforms and new levers appearing in the health reform bills before Congress. Critics complain they are too complicated. The DMCB says visit CMS outside of Baltimore and you'll understand why.
Thursday, July 30, 2009
A President's Invite for Beer as a Metaphor for Medicare's Current Coverage of Medical Necessity (Egads)
 When it comes to Medicare, beneficiaries can generally have any service that is ‘medically necessary.’
When it comes to Medicare, beneficiaries can generally have any service that is ‘medically necessary.’And when it comes to having a beer with the President, apparently you can have any brand you want, so long as it’s…beer. For Mr. Obama, it’ll be a Bud Light, while Dr. Gates prefers a Red Stripe and Mr. Crowley likes Blue Moon.
The ever curious Disease Management Care Blog knows what 'medically necessary' is, but wanted to better understand the definition of beer. It found out that it is a starch-based beverage that is commonly based on rice, wheat or barley that is fermented with one of several different types of yeast (commonly lager or ale), that is combined with a variety of hops (gives that bitter taste) and allowed to brew to various levels of alcohol concentration. Depending on the style, type and mix of the base ingredients plus other additives (for example, cherries or even hot peppers), the variety is truly endless. What’s more, beer can range from really cheap to really expensive.
Which makes it a good metaphor for health insurance coverage. The beers chosen by Mr. Obama’s guests fell within the standard ‘covered’ White House ‘benefit’ preferred by many beer drinking consumers. If Professor Gates or Mr. Crowley, however, had asked for a lusty mead or a tall glass of Strongbow, the President’s staff would have probably had to mimic a Medical Director and review the definition of ‘beer’ as well as the text of the President’s invitation. They would have determined that neither of the requests were grain-based starch beverages and therefore not covered by the invitation. Unless there was an appeal or grievance, case closed. But suppose either of the guests had chosen, based on the advice of their physician, a unique Bar Harbor or a pricey Chimay Ale? Just like Medicare, the beer would have to be served, right? Medically necessary is medically necessary and an invite for brewskies with the President is an invite for brewskies. Cheers!
The DMCB realizes it’s being silly and knows how rude it would be to abuse the gracious hospitality of a President. Decorum and common sense rule in such situations. Unfortunately, that is not the case in another corner of the Federal bureaucracy, where we as a nation have come treat the Medicare benefit as an open tab for every conceivable fermented beverage that meets the broad definition of medically necessary.
Too bad Mr. Obama can’t invite folks over for a beer when it comes to health reform. It’s all just too complicated.
Tuesday, June 30, 2009
Grandpa Harry and Grandma Louise
Word from all those town hall meetings members of Congress are having back home this week is that lots of seniors are showing up scared that all the talk of health care reform in Washington, DC might just hurt them.The seniors’ reasoning goes that Congress is getting ready to cut Medicare in order to pay for the uninsured grandkids' newfound access to a health insurance policy of their own.Watch
Sunday, April 19, 2009
Support the Patient Centered Primary Care Collaborative
The letter correctly points out that, while it was going to be difficult for small physician owned practices to participate at a Level I or II, it will be far more difficult for these clinics to attain the highest NCQA Tier III level. It takes considerable resources to attain this, and the inevitable failure to do so will effectively shut out about 1/2 of all the U.S. primary care physicians from participation. As a result, we will have no idea if the the Medical Home is a viable and generalizable option in fee for service Medicare in all corners of the country.
What are they thinking?
You're welcome to sign onto the letter to express your concern. Readers can contact Relja Ugrinic, at rugrinic@pcpcc.net, directly by COB Tuesday, April 21st, to add your name to the letter.
Subscribe to:
Posts (Atom)